How you can make a difference
Scarlett was just 13 when she had two cardiac arrests and went into end stage heart failure. Her parents were told a heart transplant was the Sydney school girl's only chance of survival. This is her story.
Scarlett was diagnosed with heart disease when she was just 10 years old.
Initially, doctors had no idea what was wrong.
“I couldn’t walk far and was always out of breath,” Scarlett recalls. “I couldn’t keep up. I didn’t have any energy. My parents just thought I was lazy.”
However, when the Sydney schoolgirl’s heart started beating really quickly one day at school, she knew it had to be something more serious.
Eventually, after seeing multiple doctors and specialists, she was diagnosed with hypertrophic cardiomyopathy – a thickening of the walls of the heart chamber.
Scarlett’s mum Amanda was told: “There is no cure, I suggest you learn CPR.”
The next few years Scarlett lived a relatively normal life, with ongoing medical appointments. But when she was 13, Scarlett’s heart stopped beating in the middle of dance class and she collapsed.
Scarlett was implanted with an internal defibrillator at hospital and sent home. But just a couple of days later while at a friend’s house, she experienced significant arrhythmia (irregular heartbeat) and fainted again.
“I was running up the stairs and the defibrillator went off four times. I remember screaming out before an ambulance came and took me straight to Westmead.
“My heart was failing and l had two cardiac arrests. At age 13, I ended up on life support for 16 days. I had a very little chance of survival.”
Her traumatised dad Philip watched the second cardiac arrest happen.
“I remember yelling out to Dad, ‘Help me help me I don’t want to die’.”
Her parents were terrified, as they watched their daughter get placed on an ECMO heart-lung bypass machine.
Then, they were given a devastating deadline.
“They told us we have two options: we can turn off her life support and let her die, or we can try for a heart transplant,” her mum Amanda said. “They said we had 14 days.”
Currently there are not enough donor hearts for the number of people who need a transplant. In Australia, more than 100 people are waiting for heart transplants at any one time, often for up to two years.
Fortunately, eight days later, a new heart was found for Scarlett. And she became the first teenager with end-stage heart failure to undergo a paediatric heart transplant at Westmead Children's Hospital.
“The operation was over 12 hours long. She has endured a difficult and traumatic recovery but we are forever thankful,” Amanda adds.
Three years on, the 17-year-old suffers from a number of chronic illnesses as a result of her cardiac arrests and the trauma of being on life support, and she still has a long road of recovery.
“It’s been very hard,” Scarlett admits.

“My legs were so deconditioned and I had severe nerve pain in both my legs. It’s the most intense pain and burning sensation,” she recalls. “I also had to be fed by a tube through my nose, because of all the trauma my body had been through – my throat kept closing up and I kept choking on food.”
She has also been diagnosed with VH (visceral hyperalgesia) and CRPS (complex regional pain syndrome).
“CRPS is one of the most painful diseases in the world according to doctors,” Scarlett explains, with a wisdom beyond her young years.
The emotional impact has also been crippling, as she ended up missing a lot of school and has also lost friends along the way.
“I missed all of year 8 and half of year 9. I think a lot of people don’t understand what it’s like to have a chronic illness," she reveals.
“I’ve had people avoid me because they don’t know what to say.”
How you can make a difference
But Scarlett is alive and forever grateful to her donor – even writing a poem, which she has shared on social media:
“To my organ donor,
You have given me a gift that I could never repay.
Your pale or golden-brown hands will never whisk away.
Your beauty has carried to this heart,
With its beauty strokes of art, that has given me a life.
I was cold as ice at a time I needed this heart, and now its beauty has
come with its overflow of ruby red blood, pumping your love.
Thank you to my organ donor for saving my life.”
As part of her recovery, Scarlett started crocheting to pass the long hours in hospital – setting up an Instagram account 'Chronically Crochets', where she sells her crochet creations and shares more about her health journey.
Scarlett shares more about her health journey on Instagram
She also has a beautiful service dog named Scout, who has helped her recover.
One day, she hopes to become a paediatric nurse.
“The nurses made the hospital feel safe and happy even when times were hard,” she reveals. “I’m forever grateful for their kindness and hopeful attitude and making the recovery from the transplant easier.
“And I’ve decided to work harder than ever to achieve my end goal of being a paediatric nurse.
Scarlett with her mum and dad
How is HRI helping?
HRI is conducting innovative research to develop new therapies for heart failure and heart attack.
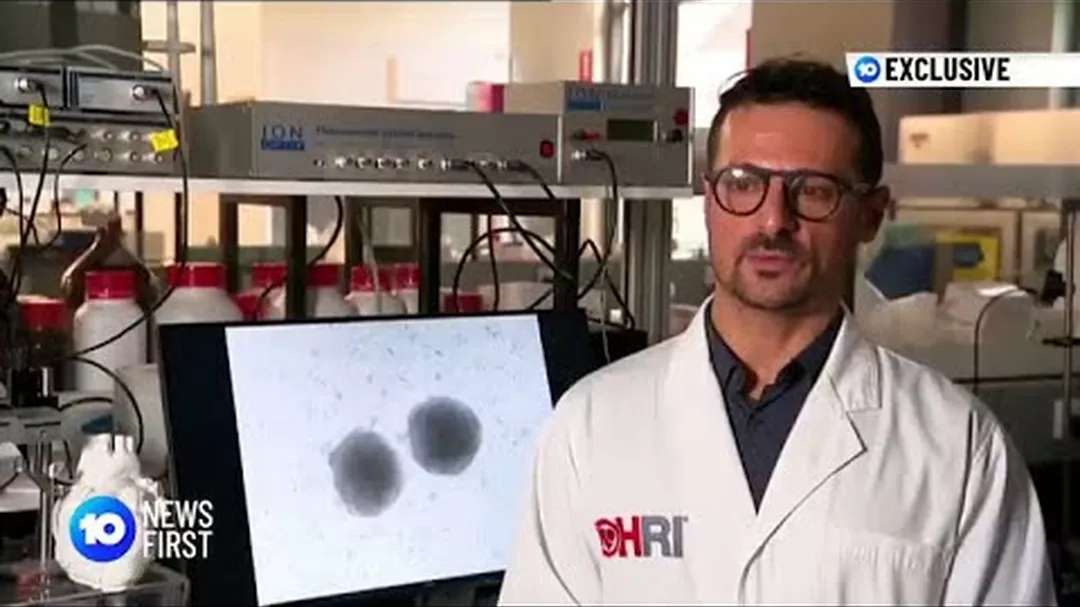
Researchers from our Cardiovascular Regeneration group, led by Dr Carmine Gentile, are working on an alternative to heart transplants using 3D-printed ‘mini-hearts’. The new technology creates personalised ‘bio-inks’ made of a patient’s own cells. These bioprinted cells form a ‘patch’, like a band-aid, which can then be used to replace the damaged tissue cause by heart failure.
Our Fluxomics Centre, led by Dr Sergey Tumanov, is devoted to identifying and exploring the cellular changes that are unique to each individual’s cardiovascular disease – with the ultimate goal of personalised methods to prevent, detect, and treat cardiovascular diseases like heart attack.
Our Coronary Diseases Group is investigating whether the anti-inflammatory drug colchicine, which has already proved safe and effective for treating conditions like arthritis and gout, can be repurposed to protect against repeat heart attacks. A collaboration between the Coronary Disease Group and our Clinical Research Group has also discovered that the heart releases certain substances during a heart attack that can be detected i