What is atherosclerosis?
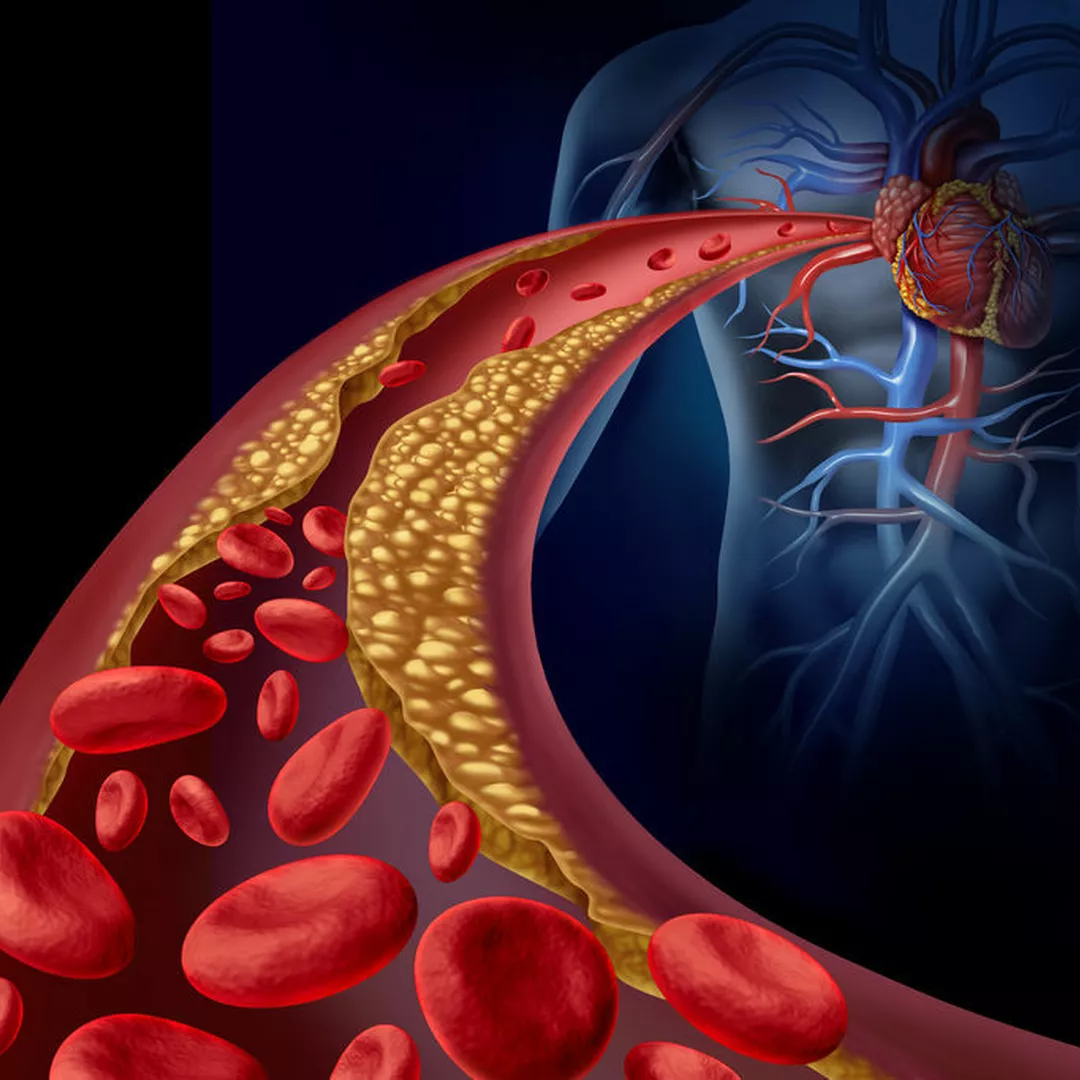
Atherosclerosis is the main underlying cause of cardiovascular disease (CVD). It is a disease in which plaques that are made up of fat, cholesterol, calcium and other substances build up in the walls of arteries.
Arteries are the blood vessels that carry blood from the heart throughout the body. They are lined with a thin layer of cells called the endothelium, which allows the blood to flow easily through the arteries. When the endothelium becomes damaged due to risk factors such as smoking or high levels of fat and cholesterol in the blood, this allows plaque to build up in the artery wall.
Over time, the plaques harden, narrow the opening of the arteries and restrict the blood flow. When these fatty plaques break open, they form a thrombus
(blood clot) that can further limit, or even block the flow of oxygen-rich blood to organs and other parts of the body.
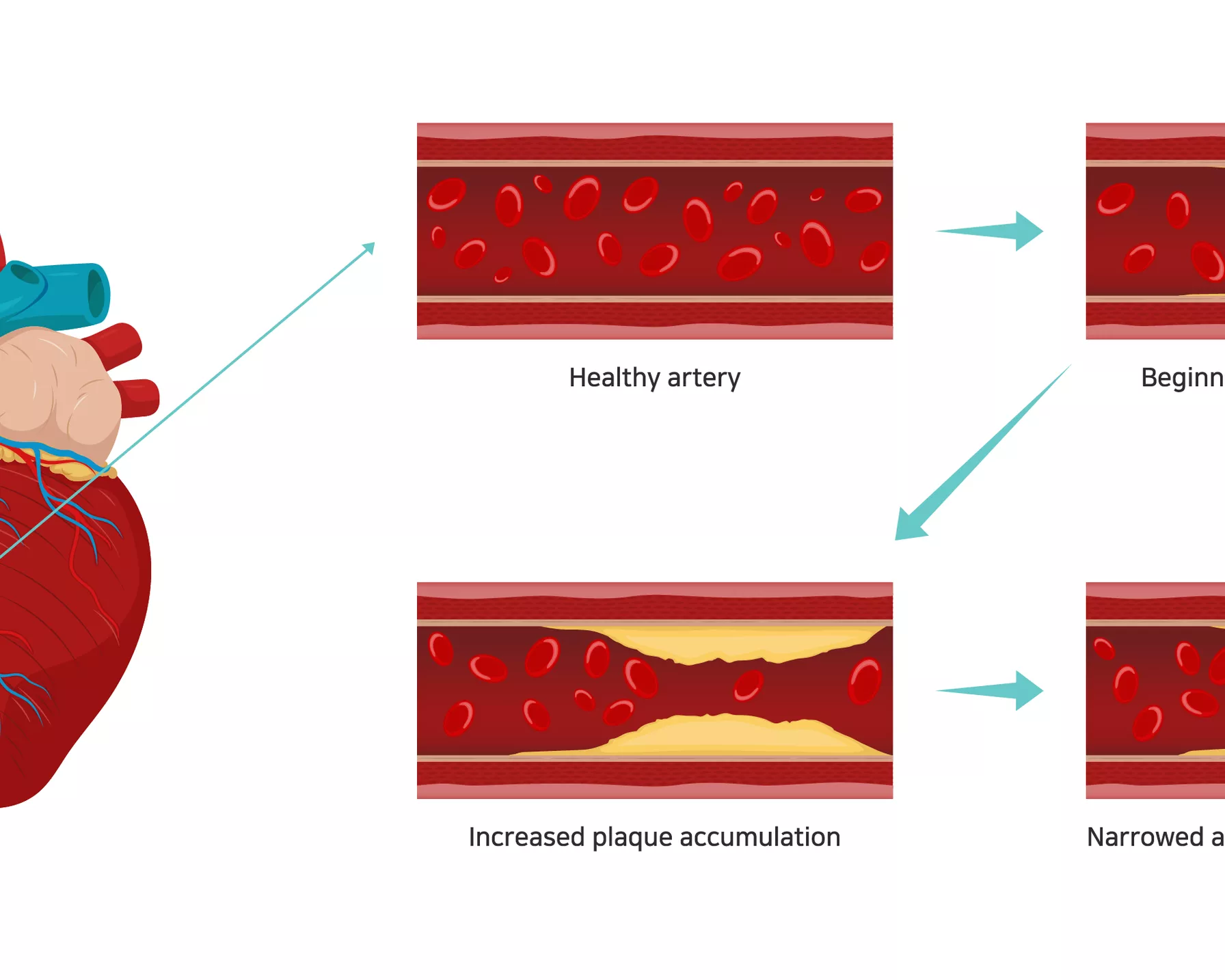
Stages of atherosclerosis. Image: iStock
Atherosclerosis can occur in arteries anywhere in the body but is most serious when it leads to a reduced or blocked blood supply to the heart or to the brain.
If it occurs in one of the two main coronary arteries that supply blood to the heart, this results in a heart attack. When thrombosis occurs in one of the arteries to the brain, it causes a stroke. If it occurs in arteries in the limbs, it can lead to peripheral artery disease.
The impact of atherosclerosis
Atherosclerosis is very common. Over the age of 40, people in general good health have about a 50 per cent chance of developing serious atherosclerosis, with this risk increasing with age. Most people over the age of 60 have some atherosclerosis, but often do not have noticeable symptoms.1
As the underlying cause of CVD – the world’s number one killer – as well as playing a key role in heart attack and stroke, atherosclerosis can have devastating and life-threatening consequences.
Atherosclerosis symptoms
Atherosclerosis usually does not cause symptoms until it is at an advanced stage, where the narrowing of arteries becomes so severe that blood flow is interrupted and cannot be carried to the organs and tissues, and CVD has developed. If the atherosclerotic plaque breaks and forms a blood clot, it can trigger a heart attack or stroke.
Within the body, a “fatty streak” is the first visible sign of atherosclerosis. This yellow streak or patch is formed from dead cells where the endothelium is damaged, and is the beginning of plaque formation. This fatty streak slowly gets bigger and forms into a larger piece of plaque.
The symptoms experienced during moderate to severe atherosclerosis depend on which arteries are affected.
- Coronary arteries (to the heart): chest pain or pressure that could lead to heart attack or heart failure if untreated.
- Carotid arteries (to the brain): symptoms of transient ischaemic attack (TIA) that may progress to a stroke if untreated – sudden weakness or numbness in arms or legs, slurred speech or difficulty speaking, temporary vision loss in an eye, or drooping face muscles.
- Peripheral arteries (to the arms and legs): symptoms of peripheral artery disease (PAD), such as decreased blood pressure in the affected limb or numbness and pain in the limbs. PAD increases the risk of stroke or heart attack, and in severe cases gangrene can occur, leading to the need for amputation.
- Renal arteries (to the kidney): high blood pressure or chronic kidney disease may develop, with symptoms such as loss of appetite, swollen hands and feet, and difficulty concentrating.
Atherosclerosis can also cause an aneurysm, where there is a bulge in the wall of the artery, anywhere in the body. While most people with aneurysms have no symptoms, there can be pain and throbbing in the area of the aneurysm. If an aneurysm bursts, life-threatening internal bleeding can occur. This is usually sudden, but a slow leak is possible. If a blood clot within an aneurysm dislodges, it could eventually block an artery.
How is atherosclerosis diagnosed?
To diagnose atherosclerosis, your doctor may take a complete family and personal medical history and also conduct a physical exam. Tests may also be administered.
- Blood tests: These can measure the amount of fat, cholesterol, sugar and protein in the blood.
- Angiogram: This type of scan uses a contrast dye injected into the arteries to help locate and measure narrowed and blocked arteries. The dye helps the blockages show up on the X-rays.
- Computerised tomography (CT) scan: This type of X-ray can show any hardening and narrowing of the large arteries in the body.
Atherosclerosis causes and risk factors
Atherosclerosis is a complex process, often starting in childhood and progressing with age. While the exact cause of atherosclerosis is not known, it may start with damage or injury to the inner layer of an artery. It is linked to certain risk factors, including a family history of CVD and increasing age, which cannot be changed. A higher risk also affects those with the following risk factors that can be managed or changed.
- High blood pressure: Medications can be prescribed to help manage high blood pressure, and dietary changes such as lowering salt intake can also help.
- High cholesterol: High levels of the “bad” cholesterol (LDL cholesterol) can be managed through medications and dietary changes.
- Obesity: Being at an unhealthy weight can increase the risk of other factors like high blood pressure and high cholesterol, which are also linked to atherosclerosis and other diseases.
- Diabetes or insulin resistance: People living with diabetes are over twice as likely to develop CVD. Some nutritional tips to help manage diabetes can help decrease the risk of atherosclerosis.
- Inactivity: Lack of exercise can contribute to being an unhealthy weight and increase the risk of high blood pressure and cholesterol levels, and atherosclerosis.
- Poor nutrition: A diet high in saturated fat, trans fat, LDL cholesterol, salt and sugar can contribute to being an unhealthy weight.
- Smoking: Smoking can damage the arteries and increase the risk of atherosclerosis.
- Stress: Stress can decrease the diameter of your blood vessels, causing an increase in blood pressure. Chronic stress is also associated with CVD.
- Sleep apnoea: This occurs when a person experiences short periods (up to 90 seconds) where breathing stops while they are asleep. It can lead to high blood pressure and put strain on the cardiovascular system.

How to prevent and treat atherosclerosis
People at risk of developing atherosclerosis should be tested if possible – early detection and the implementation of a management plan can help to prevent its progression.
Treatments for atherosclerosis aim to slow or stop plaques developing, prevent blood clots forming and treat symptoms. These can include simple lifestyle changes to manage as well as prevent the disease, such as eating a nutritious diet with minimal saturated fats, leading an active lifestyle to help maintain a healthy weight, moderating alcohol consumption, and quitting smoking.
A doctor may prescribe medications for an individual’s particular health condition and risk factors, such as drugs to help manage high cholesterol and blood pressure levels, as well as drugs to prevent blood clots and inflammation.
In severe cases of atherosclerosis, surgery may be conducted to ensure that blood can continue to flow effectively through the arteries. These include procedures such as the insertion of a stent to widen the artery, bypass surgery to carry blood around the affected area, and surgery to remove plaque build-up.
Speak to your doctor if you are concerned about your risk of atherosclerosis.
How is HRI fighting atherosclerosis?
HRI is conducting groundbreaking research from a broad range of angles to understand how atherosclerosis develops and to find innovative ways of preventing, detecting and treating the resultant CVD.
Importantly, our Vascular Complications Group has discovered a new class of white blood cells that protect against atherosclerosis, and they are now trying to find a way of boosting these cells in models of CVD.
References
- Tuzcu EM et al; High Prevalence of Coronary Atherosclerosis in Asymptomatic Teenagers and Young Adults; Circulation. 2001;103:2705–2710.