What are blood clots?
Blood clots form when blood thickens, forming a semisolid mass. They normally only form if a blood vessel is injured, such as if there is a cut to the skin, and bleeding starts. The blood thickens and forms a clot at the site of the cut to stop the bleeding.
Blood clots can happen if the blood starts to clot more easily (eg, if a person is unwell), if there are changes to the walls of the veins (eg, as a result of a long period of sitting), or if there are changes in how the blood flows.
Blood clotting (coagulation) is an important, natural process that occurs to prevent excessive bleeding, and normally the blood clot will naturally dissolve after the injury has healed.
However, blood clots can also form on the inside of blood vessels that don’t have an obvious injury, and some may not dissolve naturally. A blood clot forming inside a blood vessel is known as thrombosis.
An immobile blood clot attached to the inside of a blood vessel is generally not harmful. However, such a blood clot can become dangerous if it breaks free and travels through the blood vessels, as it could become lodged and block blood flow.
If a blood clot blocks blood flow to the heart, it can lead to a heart attack. If it occurs in an artery to the brain, it can cause a stroke. If it occurs in arteries in the limbs, it can lead to peripheral artery disease.
How do blood clots form?
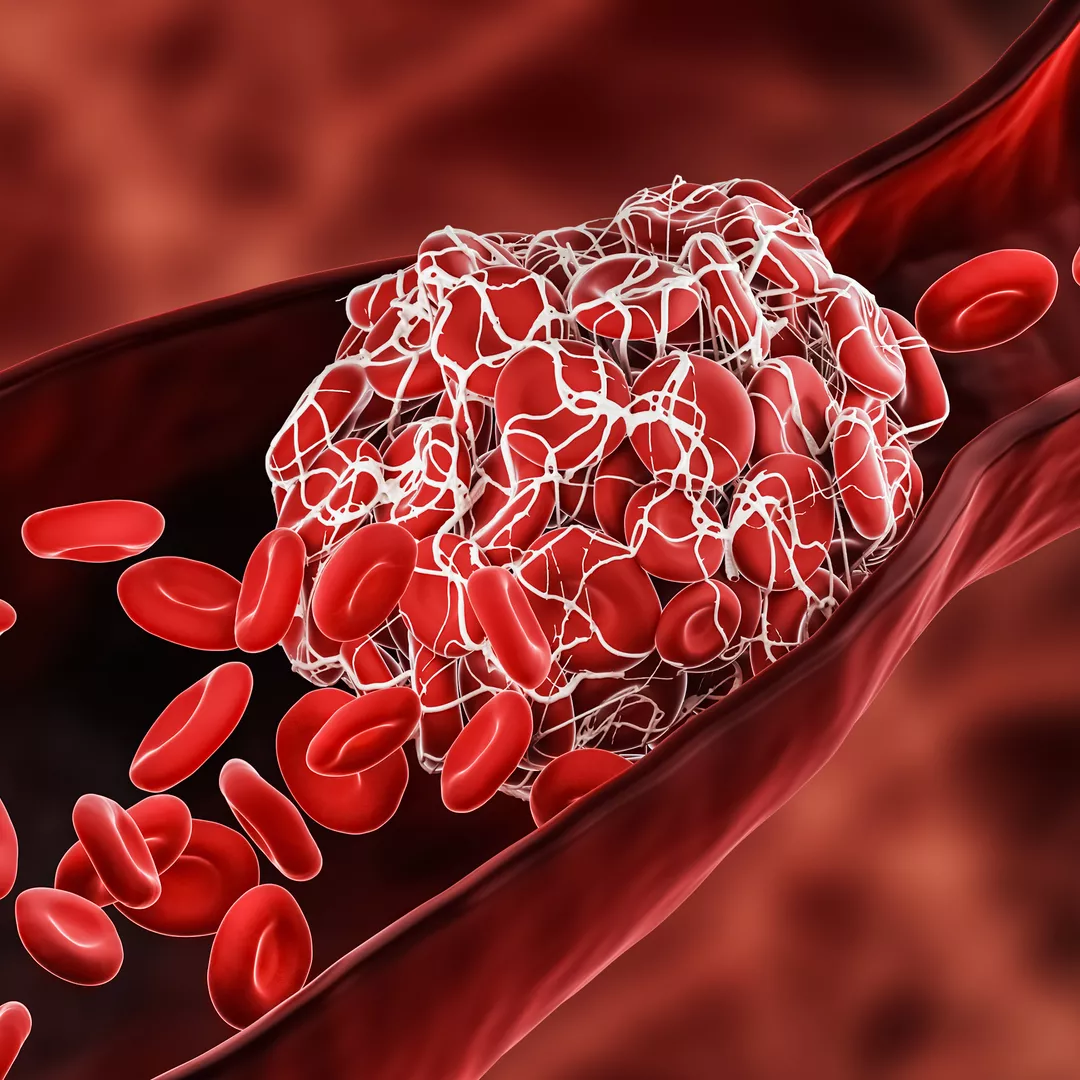
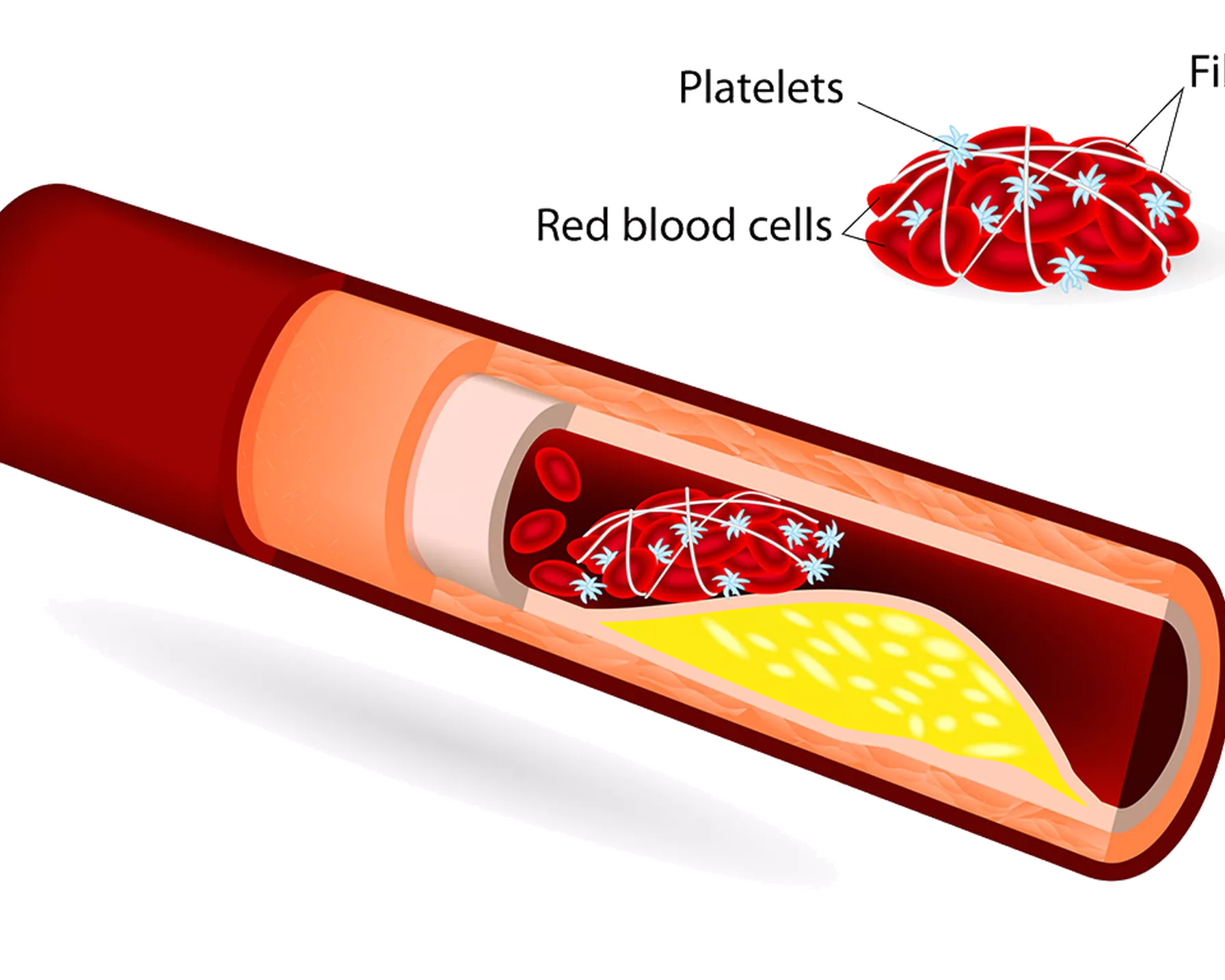
Blood clots form when blood clotting cells – known as platelets – are triggered to stick to each other, and to diseased or damaged blood vessels. These blood clot “road blocks” are secured in place by strands of fibrin, likened to mortar securing in place bricks (platelets) to create a solid and secure blood clot in the blood vessel.
Blood clots are formed from red blood cells, platelets (blood clotting cells) and fibrin. They can block arteries and become dangerous.
Blood clot causes
Unwanted blood clots within blood vessels (thrombosis) can form as a result of atherosclerosis. In this slow, progressive process, atherosclerotic plaques that are made up of fat, cholesterol, calcium and other substances build up in the walls of the arteries. Over time, these plaques harden, narrow the opening of the arteries and restrict the blood flow. If these plaques break open, they form a blood clot.
Atherosclerosis is the main underlying cause of cardiovascular disease (CVD).
Types of blood clots
There are two main types of blood clots depending on which blood vessels are blocked.
Arterial blood clots
These are when a blood clot blocks an artery. Blood clots in the arteries can be dangerous, as the arteries carry oxygen- and nutrient-rich blood from the heart around the body. The clots can prevent oxygen and nutrients from reaching essential organs like the brain.
Venous blood clots
These are when a blood clot blocks a vein. Veins carry deoxygenated blood away from the body’s organs back to the heart. A blood clot in a vein can restrict the return of blood to the heart, resulting in serious problems.
Superficial blood clots
These occur in a vein near the skin. While they can be painful, they are usually not serious.
Problems caused by blood clots
Blood clots in the heart
Blood clots in the heart can block critical blood flow and result in a heart attack (also known as a myocardial infarction). If the blockage stops blood flow to the heart, the amount of oxygen that the heart receives is reduced. Without oxygen, the heart muscle can start to die. The longer that the blockage remains untreated, the greater the damage to the heart. Without treatment to restore blood flow, the heart can be permanently damaged.
Blood clots in the brain
A blood clot in the brain can block the supply of oxygen-carrying blood to the brain, causing a stroke. Brain tissue starts dying without a constant supply of oxygen, so it is critical to treat the stroke as soon as possible. The longer a stroke remains untreated, the greater the chance that brain cells will die, leaving behind permanent stroke-related brain damage. These debilitating effects can include weakness on one side of the body, difficulty controlling movements, personality or behaviour changes, or problems speaking and understanding.
Blood clots in the legs
A blood clot in the limbs can lead to peripheral artery disease (PAD). While PAD is not immediately life threatening, someone with PAD has a greatly increased risk of having a heart attack or stroke. The reduced blood flow to the limbs can also lead to the limb developing gangrene, where it starts to decay and die. The only treatment option for gangrene is to amputate the affected limb to prevent the gangrene from spreading further in the body.
Blood clots can also cause deep vein thrombosis (DVT), which most commonly affects major veins in the leg. In DVT, there is the risk that a clot breaks off, travels through the blood stream, and becomes lodged in the pulmonary artery (the main blood vessel to the lungs). This is known as a pulmonary embolism and can be extremely dangerous. DVT can also occur in the arms, pelvis or other large veins in the body, but this is less common.
Blood clot symptoms
The signs and symptoms of blood clots will vary depending on where the clot is located, and they may appear similar to symptoms of other conditions. It is also possible to have a blood clot with no apparent symptoms.
It’s important to know the signs to look out for, but only a healthcare professional can confirm whether you have a blood clot. They will do so by looking at your symptoms and medical history, and they may also order tests, such as an ultrasound to show an image of your blood vessels.
Signs of blood clots: how do you know if you have a blood clot in the heart?
Symptoms of blood clots in the heart can include chest pain, light-headedness, discomfort in other areas of the upper body (such as the neck, back, jaw or arm), shortness of breath, sweating or nausea.
Signs of blood clots: how do you know if you have a blood clot in the brain?
Symptoms of blood clots in the brain are the same as the symptoms of a stroke. These can include numbness or weakness in the arm, face or leg (especially on one side of the body), slurred speech or trouble speaking or understanding others, dizziness or a sudden, severe headache, or vision problems.
Signs of blood clots: how do you know if you have a blood clot in the arm or leg?
Symptoms of blood clots in the arm or leg can range from mild to severe, depending on the size of the clot. These can include swelling, sudden or gradual pain, tenderness or a warm sensation in the location of the clot.
The risk of blood clots
Blood clots are common, and in general they can be harmless. The risk factors for developing a blood clot in an artery versus a vein are different, and people may be at risk of one but not the other. Usually there is a combination of factors that leads to a blood clot, but you are more likely to develop a blood clot if you:
- have other medical conditions that make clotting more likely, such as a blood disorder, heart condition or diabetes
- do not move around or are immobile for a long period of time, such as through hospitalisation or sitting on a long-haul flight
- have had surgery or a major injury, especially to the legs
- have had a blood clot before or a family history of blood clots
- are on certain medicines that may increase your risk of clotting or that contain oestrogen, such as birth control and hormone replacement therapy
- are pregnant or six weeks post-birth
- have varicose veins
- are over 50, as age can increase the body’s natural ability to clot.
Certain lifestyle factors also increase your risk of blood clots. These include:
- being inactive in general
- being overweight or obese
- having high blood pressure or high cholesterol
- smoking
- being dehydrated.
Preventing blood clotting
Making small adjustments to your lifestyle can help to decrease your risk of developing a blood clot.
- Maintain a healthy weight by eating heart-healthy, nutritious food.
- Keep physically active – stay motivated by choosing the best exercise for your life stage.
- Avoid long periods of inactivity or sitting by taking regular breaks to move around.
- Manage high blood pressure and control cholesterol levels through medication and diet, in consultation with a healthcare professional.
- Stay well-hydrated, as dehydration can contribute to the development of blood clots.
To prevent blood clots from forming, a doctor may prescribe blood thinning or anticoagulation medication to thin the blood and make it less likely to clot.
Blood clot treatment
How a blood clot is treated will depend on its type, its location and your overall health condition.
Medication may be prescribed to thin the blood and make it less likely to clot, preventing blood clots from forming (anticoagulants). There is also medication available to dissolve blood clots (thrombolytics). In some cases, surgical procedures may be necessary, such as a thromboectomy to remove a blood clot.
How is HRI fighting blood clots?
HRI is conducting groundbreaking research from a broad range of angles to understand blood clots and the potential cardiovascular disease that can result.
Our Vascular Complications Group is investigating ways to stimulate blood vessel growth to bypass arteries blocked by blood clots in peripheral artery disease.