Stroke definition: what you need to know
A stroke (also known as a cerebrovascular accident) occurs when the brain does not get the blood supply that it needs, such as through the blockage or rupture of an artery.
Blood carries oxygen and important nutrients around the body for proper functioning. If brain cells and tissue do not get enough blood supply, they become damaged and die. Brain cells can die very quickly without enough blood – up to 1.9 million brain cells can die every minute.
Early treatment for stroke is critical – the longer a stroke remains untreated, the greater the chance of stroke-related brain damage.
There are two major types of stroke: ischaemic and haemorrhagic. An ischaemic stroke is when blood flow to the brain is interrupted, eg, when a blood clot blocks a brain artery. A haemorrhagic stroke is when a blood vessel or artery in the brain bursts, and there is a leakage of blood into the brain. Both types of stroke share the same possible signs, symptoms and effects.
What is the difference between a stroke and transient ischaemic attack?
A transient ischaemic attack (TIA), sometimes called a ministroke, happens when blood supply to the brain is blocked for a short time. TIAs show the same signs and symptoms as a stroke, but these often only last for a few minutes and then go away when the blockage moves and blood flow is restored.
TIAs indicate that a full stroke may happen, so it is important to seek emergency medical attention if you experience any of the symptoms, even if they go away. With early identification of symptoms and early management by healthcare professionals, the chance of a major stroke is greatly reduced.
What can cause a stroke?
The two main types of stroke – ischaemic and haemorrhagic – have different causes.
What causes ischaemic stroke?
An ischaemic stroke is caused by atherosclerosis. In this process, fat, cholesterol and other substances build up and form plaque in the arteries, which can narrow them. This plaque can form a blood clot (thrombosis) that can break away from the artery wall and block blood flow. If this blockage occurs in the arteries leading to the brain and stops part of the brain from receiving blood, the result is a stroke.
Ischaemic stroke makes up almost 90 per cent of strokes.
There are two types of blockages that can cause different types of ischaemic stroke.
- Cerebral embolism: This occurs when a blood clot forms elsewhere in the body, most commonly in the heart, and travels through the bloodstream to the brain. If the clot reaches an artery in the brain that is too narrow for it to pass through, it gets stuck and stops blood from getting through. This causes an embolic stroke.
- Cerebral thrombosis: This occurs when atherosclerotic plaque builds up in the arteries to such an extent that the artery is narrowed and blocked, causing a thrombotic stroke. In this type of stroke, this most commonly occurs in the major arteries in the neck that carry blood to the brain.
What causes haemorrhagic stroke?
A haemorrhagic stroke occurs when a blood vessel or artery in the brain breaks open, causing leakage of blood into the brain and stopping the delivery of oxygen and nutrients. This is also called a cerebral haemorrhage. The blood from the burst artery also creates excess pressure in the head and swells the brain, which can damage the brain cells and tissues.
Haemorrhagic strokes can be caused by high blood pressure, defects in the blood vessels, or an aneurysm (a weak or thin spot in the wall of an artery that can get weaker and burst).
Blood-thinning medications such as anticoagulants (which are taken to lower the risk of blood clots) can increase the risk of haemorrhagic stroke, as can some illegal drugs.
Ischaemic stroke occurs when blood supply to the brain is cut off by a blood clot. Haemorrhagic stroke occurs when a blood vessel or artery in the brain bursts, leaking blood into the brain.
Stroke symptoms
In a stroke, parts of the brain do not get the blood supply and oxygen they need, so brain cells and tissues become damaged and start to die. The body parts that are controlled by the damaged areas of the brain will be affected and show signs of stroke.
The most common signs and symptoms of stroke are:
- facial weakness
- arm weakness
- difficulty with speech.
Other symptoms of stroke that may occur include:
- weakness, numbness or paralysis of the face, arm, or leg on either or both sides of the body
- slurred speech or difficulty understanding
- loss of vision in one or both eyes
- sudden, severe headache or a change in pattern of headaches with no known cause
- loss of balance, dizziness.
The signs and symptoms of stroke may occur alone or in combination. These can last a few seconds or even up to 24 hours and then disappear (as in the case of TIAs).
Recognising stroke
An easy way to recognise and remember the signs of stroke is to use the FAST test. If someone is showing these symptoms, immediately seek emergency medical treatment.
- Face: Check whether their facial features, such as their mouth, have drooped.
- Arms: Can they lift both arms?
- Speech: Are they having difficulty speaking, eg, slurring their speech? Can they understand you?
- Time: Time is critical if you see any of the above signs. Call emergency services immediately.
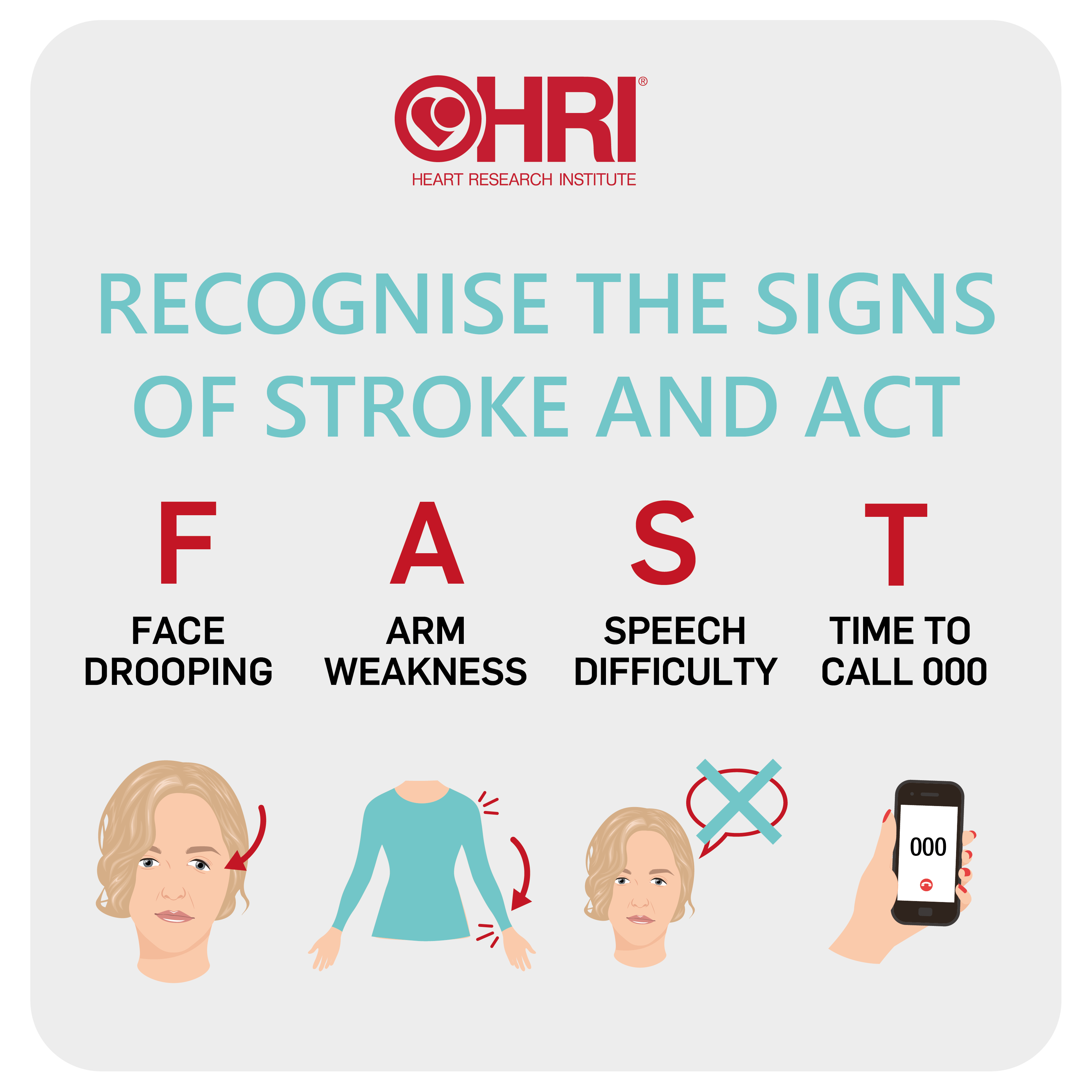
Stroke is a medical emergency – the longer that a stroke remains untreated, the greater the chance of stroke-related brain damage.
Complications of stroke
Every stroke is different, and each person who suffers a stroke will be affected in different ways. Stroke can cause permanent or temporary disabilities, and in some cases can be fatal. The longer that a stroke remains untreated, the greater the chance of brain damage and lasting complications. That’s why it’s so important to develop new treatments and therapies for stroke.
The effects and complications that can result from stroke will depend on which part of the brain was affected by the stroke, as the four different parts of the brain control different parts and functions of the body.
Stroke in the right side of the brain
The right side of the brain controls perception and the left side of the body, among other things. A stroke affecting this side of the brain can cause issues such as:
- short-term memory loss
- inability to judge distances, which can lead to loss of coordination and falls
- impulsive behaviour
- paralysis of the left side of the body.
Stroke in the left side of the brain
The left side of the brain controls speech and the right side of the body, among other things. A stroke affecting this side of the brain can cause issues such as:
- short-term memory loss
- speech and communication problems
- paralysis of the right side of the body.
Stroke in the cerebellum
The major functions of the cerebellum in the brain include control of coordination and balance. A stroke affecting this part of the brain can cause issues such as:
- loss of coordination and balance
- dizziness and a tendency to fall
- nausea and vomiting
- slurred speech.
Stroke in the brain stem
The major functions of the brain stem include control of breathing, heart rate and blood pressure. A stroke affecting this part of the brain can cause issues such as:
- paralysis of the whole body
- coma
- death.
The impact of stroke
Every 19 minutes, one Australian experiences a stroke for the first time, and almost half a million Australians live with the effects of stroke. Without action and further research into preventing and treating stroke, by 2050 this is predicted to increase to one stroke every 10 minutes, with one million Australians living with the lasting effects of stroke.1
Survivors are likely to suffer a decreased quality of life for many months, if not years, post-stroke. They may need long-term rehabilitation as well as the support of family, loved ones and other carers and healthcare professionals. Sadly, around one in five people will die within 28 days of a stroke, and one in three people will die within a year.2
Stroke also places a huge burden on the healthcare system – the financial cost of stroke in Australia is estimated to be $6.2 billion each year.1
Over 90 per cent of people who have a stroke remain without effective treatment and must suffer the debilitating consequences, as the only clinically approved drug to treat ischaemic stroke can be used in only a small percentage of patients due to its severe side effects. To address this urgent need, the Heart Research Institute is conducting a world-first trial of a new anti-clotting drug that could potentially be used in all people who suffer a stroke.
Main risk factors for stroke
There are several factors that increase your risk of stroke that can be controlled or treated. The most important ones are the following.
High blood pressure and risk of stroke
High blood pressure can lead to stroke by damaging blood vessels walls and making them weaker, and by causing blood clots to break off and block arteries to the brain. It is the leading risk factor for stroke – the higher the blood pressure, the greater the stroke risk.
However, high blood pressure can be managed and controlled through dietary changes like lowering salt intake, as well as by leading a healthy lifestyle.
It’s important to know your blood pressure levels and keep them at a healthy level. Your doctor can help regularly check your blood pressure, and home measurement devices are also available.
Atrial fibrillation and risk of stroke
One in every three strokes is linked to atrial fibrillation (AF), a condition where the heart beats irregularly or rapidly. People with AF are at increased risk of ischaemic stroke, and AF-linked strokes are more severe than other strokes.
AF can remain undetected for long periods of time, which is why it is important to screen for AF to prevent potential stroke.
Once detected, AF can be managed though medications that help reduce the risk of blood clots as well as treatments and medical procedures to help the heart beat slower or more regularly.
Other risk factors for stroke
Other risk factors for stroke that can be controlled include the following.
- High cholesterol: High levels of LDL cholesterol, the “bad” cholesterol, can increase the build-up of atherosclerotic plaque. Making dietary changes can help manage high cholesterol, as can leading a healthy lifestyle. Medications to manage cholesterol levels are also available.
- Smoking: Smoking doubles the risk of stroke, and the more that is smoked, the greater the risk. This is because smoking can increase blood pressure, as well as damage the blood vessels and heart, leading to stroke and other cardiovascular diseases. The risk of a stroke or heart attack drops immediately after a person quits smoking; the risk can drop by up to half after one year.
- Overweight and obesity: Being overweight or obese increases the risk of stroke, as well as the risk of high blood pressure, high cholesterol and cardiovascular diseases. To reach and maintain a healthy weight, try to eat a healthy diet and exercise regularly.
- Excessive alcohol intake: High levels of alcohol consumption can increase blood pressure, and people who drink heavily are three times more likely to have a stroke.
- Poor nutrition: A diet high in saturated fat, trans fat, LDL cholesterol, salt and sugar can contribute to being an unhealthy weight and increase the risk of high cholesterol and high blood pressure. Eating a balanced, nutritious diet can help maintain a healthy weight and support optimal health.
- Inactivity: Being inactive can increase the risk of high blood pressure, high cholesterol and being an unhealthy weight. It is also important to stay active after a stroke, even if you have mobility difficulties, under the guidance of a healthcare professional.
- Diabetes: The risk of having a stroke doubles for people with diabetes compared to those without. It is important to keep diabetes under control by monitoring blood sugar levels and keeping them within the range recommended by your healthcare professional through medications, dietary changes and regular exercise.
Risk factors for stroke that cannot be controlled include age (being over 65 years of age), gender (women have higher risk of fatal stroke) and a family history of stroke. People who have previously had a stroke are also at increased risk of having another.
Women and stroke
Cardiovascular disease can affect women differently. While stroke occurs in both men and women, more women have strokes than men, and more women than men die of stroke.
Women tend to have strokes when they are older, when the impact can be more devastating and more disabilities may occur. Women also bear more of the long-term burden of stroke.
There is a higher lifetime risk of stroke for women, with risk factors specific to women on top of the risk factors for both men and women. The increased risk in women is associated with the following.
- Oral contraceptive pills: Some types of pill can increase the risk of blood clots, and so increase the risk of stroke.
- Pregnancy: Although not common, pregnancy is a risk factor, especially if preeclampsia or high blood pressure are also present. Hormonal factors during pregnancy can also increase the risk of blood clots.
- Migraines: Experiencing migraines with visual side effects, such as flashing lights and difficulty focusing on things, is a risk.
How to prevent stroke
More than 80 per cent of strokes can be prevented by managing your risk factors and leading a healthy, active lifestyle.
The first step is to see your doctor to have a health check and find out whether your blood pressure and cholesterol levels are within a healthy range. Dietary choices and medication can help to control high blood pressure or lower cholesterol levels.
Your doctor can also help determine your risk of type 2 diabetes and atrial fibrillation, or if you have them, help to manage and treat them.
You can also make positive lifestyle changes to help reduce the risk of a stroke and to help control the factors that can increase the risk of stroke.
- Eat a heart-healthy, balanced diet that is low in saturated fats and that includes a variety of fruit, vegetables, wholegrains and healthy protein sources.
- Exercise regularly to help maintain a healthy weight.
- Limit alcohol intake, as this can increase blood pressure and triple the risk of stroke.
- Quit smoking as it can damage the arteries and double the risk of stroke.
Speak to your doctor for advice and support specific to your health.
How is stroke diagnosed?
It is vital to call emergency services immediately if you or someone you know show any of the signs and symptoms of stroke. Paramedics can assess you for stroke and get you to the hospital for emergency diagnosis and treatment.
Doctors will conduct some tests to confirm that the symptoms are due to stroke, determine the type of stroke, and find out what area of the brain was affected as well as how severe the impact of the stroke was on the brain. The aim is to discover the cause of the stroke and start treating it.
The tests may include:
- brain scans, such as computerised tomography (CT scan) and magnetic resonance imaging (MRI), to show what areas of the brain have been damaged and help determine whether the stroke was ischaemic or haemorrhagic
- heart tests, such as an electrocardiogram (ECG), which can determine whether there is any heart condition that may have led to the stroke
- blood tests to rule out other health conditions and help determine the best treatment for the stroke.
Stroke treatment
Stroke is a medical emergency, and immediate treatment is critical. The longer a stroke remains untreated, the greater the chance of stroke-related brain damage.
The type of stroke treatment or stroke medication depends on the type of stroke.
How is ischaemic stroke treated?
Blood clots or blockages in the brain cause this type of stroke, so treatments are aimed at removing the blood clot and restoring blood flow to the brain, to minimise the damage caused by the stroke.
There are two emergency treatments for ischaemic stroke.
- Thrombolysis: This is when a clot-busting drug is used to break down blood clots. There is currently only one effective drug, called tissue plasminogen activator (TPA). However, TPA must be used within four and a half hours of the stroke to be effective and has a high risk of dangerous side effects, including severe bleeding and further clotting. This means it can only be administered to around 10 per cent of ischaemic stroke patients – up to 90 per cent of people who suffer an ischaemic stroke cannot receive this emergency treatment and are at risk of suffering life-long disabilities from the stroke.
- Thrombectomy: This surgical procedure uses a device to pull the blood clot out of the blood vessel and is often used together with thrombolysis. It is most successful if performed within six to 24 hours after a stroke.
There is an urgent need to find a way to extend the treatment window for ischaemic stroke and to make treatment safer, so that more people who suffer an ischaemic stroke can be treated. To that end, HRI is conducting a world-first trial of a new anti-clotting drug that could potentially be used in all people who suffer a stroke.
How is haemorrhagic stroke treated?
This type of stroke is due to bleeding in the brain, so the main goal of treatment is to help the blood clot, to stop the bleeding.
Treatment depends on the location and severity of the haemorrhage. This may include medications to counteract any blood-thinners being taken and to lower blood pressure or treat underlying causes, and medical procedures or surgery to reduce and prevent further bleeding.
How is HRI fighting stroke?
HRI is tackling the devastating impact of stroke from a broad range of research angles.
Our Heart Rhythm and Stroke Prevention Group is investigating how best to screen at scale for atrial fibrillation (AF), which is linked to one third of strokes, to prevent as many strokes as possible. With a clinical implementation focus, the Group is exploring novel strategies using eHealth tools and patient self-screening to detect unknown silent AF. If screening for AF could be implemented more widely in people aged 65 and older, along with preventative treatments being prescribed as advised in guidelines, then thousands of strokes could be avoided globally, making a difference to patients and their families.
Our Cardiovascular-protective Signalling and Drug Discovery Group is researching a rapid, non-invasive treatment for ischaemic stroke by developing a cutting-edge technological platform for photo-responsive stroke therapy. This research will provide proof-of-concept information on the utility of this photo-pharmacology system in the treatment of thrombosis and stroke for the first time.
Stroke: what you need to know
References
- Deloitte Access Economics. No postcode untouched – Stroke in Australia, 2020.
- Thrift AG et al; Stroke Incidence on the East Coast of Australia: The North East Melbourne Stroke Incidence Study (NEMESIS), 2000 Stroke, 31: 2087-2092.
- Deloitte Access Economics. The economic impact of stroke in Australia, 2020.