What is preeclampsia in pregnancy?
Preeclampsia is a serious condition where high blood pressure develops during pregnancy, affecting both the mother and unborn baby. There may also be high levels of protein in the mother’s urine (proteinuria), which indicates kidney damage, and other signs of organ damage.
Preeclampsia puts stress on the heart and other organs and is associated with a number of serious effects, including kidney dysfunction, swelling of hands, feet and face, dizziness, headaches and difficulties with vision. It also increases the risk of the mother developing cardiovascular disease or other heart conditions in the future.
If untreated, preeclampsia can lead to serious complications such as convulsions, kidney or liver failure, and blood clotting problems. In severe cases, preeclampsia can lead to maternal and infant death. In some cases, the baby needs to be delivered early.
Preeclampsia usually resolves after the baby is born and the placenta is delivered, and the mother’s blood pressure usually returns to normal.
What is postpartum preeclampsia?
Postpartum preeclampsia is when preeclampsia develops after the baby is delivered. It typically develops within 48 hours of childbirth but can occur at any time up to six weeks after the baby is born. It shows most of the same signs and symptoms of preeclampsia in the mother, eg, high blood pressure, but does not affect the baby.
Can preeclampsia affect the baby?
Preeclampsia affects the arteries that carry blood to the placenta, which is the organ that provides oxygen and nutrients to the baby in the womb from the mother’s blood.
High blood pressure in preeclampsia can decrease the amount of oxygen and nutrients getting to the placenta and to the baby, which in severe cases can starve the baby and affect its growth. This growth restriction can put the baby at risk, and the baby may need to be delivered early or prematurely. This increases the risk of the baby having health complications such as low birth weight, problems with its breathing, feeding, vision and hearing, as well as developmental delays.
Preeclampsia symptoms and signs of preeclampsia
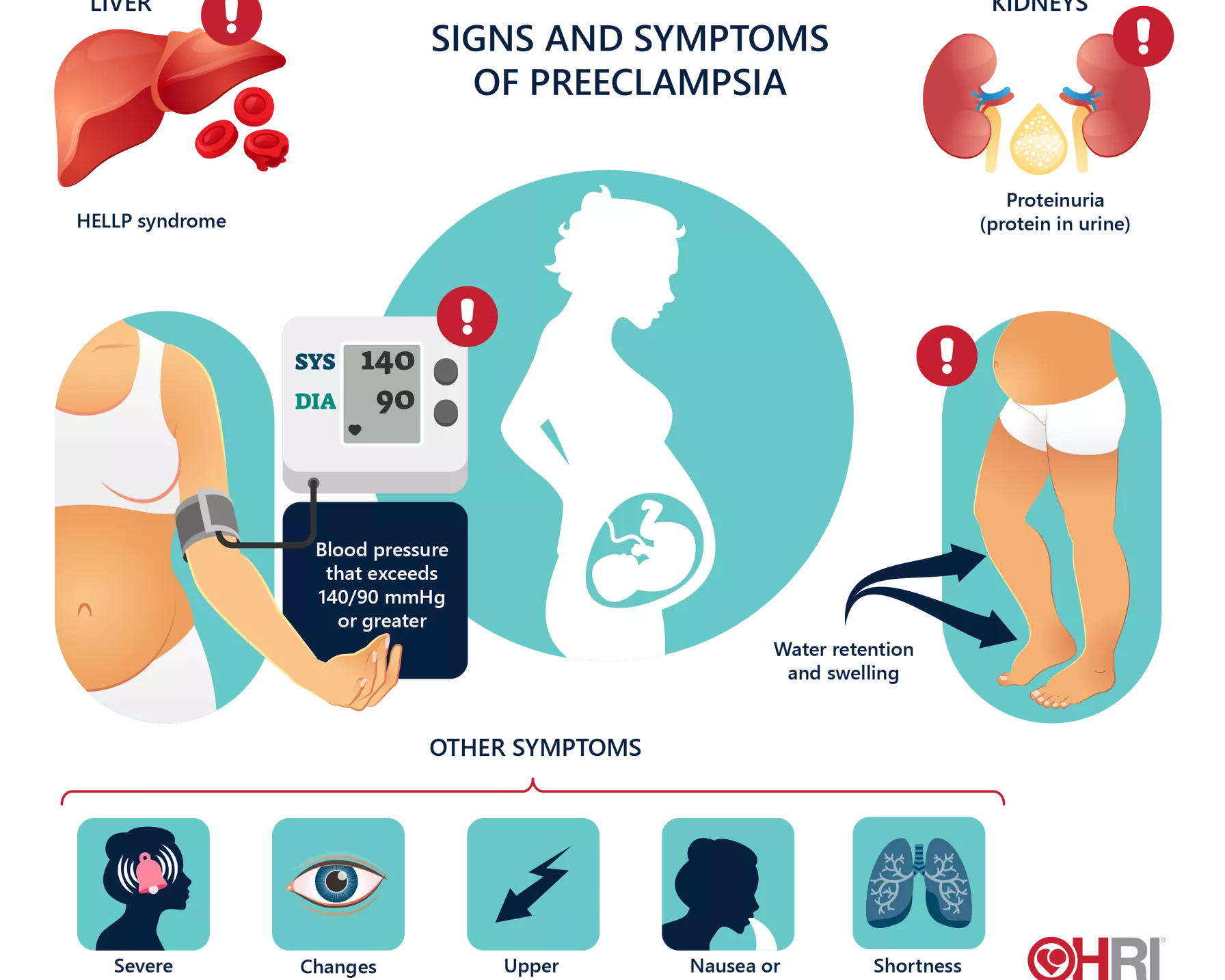
The defining sign of preeclampsia is high blood pressure and high levels of protein in the urine, both of which may not show immediately noticeable signs. The severity of preeclampsia is determined by the level of blood pressure.
Preeclampsia: early signs and symptoms
Initially, preeclampsia has no obvious symptoms, and most women with the condition feel normal and well. The first signs of preeclampsia are often detected during routine prenatal visits with a healthcare professional, which is why regular check-ups during pregnancy that include blood pressure checks are so important.
Early signs and symptoms of preeclampsia include:
- a sudden rise in blood pressure so that levels exceed the initial level at the start of pregnancy
- excess protein in the urine, which can be a sign of kidney damage.
Preeclampsia: advanced signs and symptoms
Over time, preeclampsia can cause fluid retention (oedema). Oedema is a common occurrence during pregnancy, usually causing swelling around the feet and ankles. However, sudden swelling of the face, hands or feet may be a sign of preeclampsia. Sudden weight gain could also be an indicator.
Some of the other signs and symptoms of preeclampsia include:
- headaches
- changes in vision and visual disturbances, such as blurred vision or light sensitivity
- shortness of breath
- pain in the abdomen, usually in the right side just below the ribs
- nausea and vomiting
- decreased levels of platelets in the blood
- increased liver enzymes that indicate liver problems.
If you have severe headaches, blurred vision, severe pain in the stomach or severe shortness of breath, contact your doctor or emergency services immediately.
Preeclampsia complications
Preeclampsia can lead to serious complications that could threaten the lives of both mother and baby if left untreated.
Preeclampsia increases the risk of placental abruption, where the placenta separates from the wall of the uterus before delivery. This can cause heavy bleeding that can be dangerous for both mother and baby.
The risk of HELLP syndrome (haemolysis, elevated liver enzymes and low platelet count), a severe form of preeclampsia that affects several organs, is also increased. HELLP can be life-threatening to mother and baby, and cause life-long health problems for the mother.
Eclampsia, severe preeclampsia that causes seizures, is a complication of preeclampsia that can happen without signs of preeclampsia. In rare cases, it can lead to coma, stroke or even death.
The development of the baby in the womb may be restricted by preeclampsia. Early or premature delivery of the baby to treat preeclampsia can also impact the baby’s development.
After the baby is born, the mother may be at increased risk of:
- cardiovascular disease
- heart attack
- stroke
- kidney disease
- developing preeclampsia in future pregnancies.
The impact
Every year, 10,000 women in Australia are diagnosed with preeclampsia. Worldwide, around 76,000 pregnant women die each year from preeclampsia and related disorders.1
The impact of preeclampsia is not confined to just pregnancy. Women diagnosed with preeclampsia have over twice the long-term risk of cardiovascular disease and stroke compared to women without.2
Preeclampsia is a major cause of pre-mature birth, and a strong contributor to stillbirths and newborn deaths, claiming the lives of nearly 500,000 babies worldwide every year.1
How common is preeclampsia?
Preeclampsia is the most common serious medical complication of pregnancy, affecting one in every 10 women during pregnancy.3 It is more common in first pregnancies.
Preeclampsia causes
The exact cause of preeclampsia is not known, but it is thought to occur when there is a problem with the placenta. The blood vessels of the placenta fail to develop normally, and toxic proteins are released into the mother’s bloodstream. This leads to constriction of the blood vessels and damage to their lining, which causes blood vessel dysfunction. This process can affect many other bodily systems, including the circulatory system, kidneys, brain, liver and lungs. There is also thought to be a genetic component.
HRI is investigating preeclampsia to better understand its causes and to discover new, safe treatments that would allow pregnancies with preeclampsia to progress to full term.
Preeclampsia risk factors
Women who may be more at risk of preeclampsia include those who:
- are pregnant for the first time
- have pre-existing high blood pressure
- have diabetes
- are overweight or obese
- have an autoimmune disorder
- are pregnant with more than one baby
- used vitro fertilisation to become pregnant
- have had preeclampsia in a previous pregnancy
- have a family history of preeclampsia
- are over the age of 40.
How quickly can preeclampsia develop?
Preeclampsia generally develops after 20 weeks of pregnancy, although it can develop at any time during the second half of the pregnancy. It most commonly develops at or near the term of the pregnancy.
How to prevent preeclampsia
If you have risk factors for preeclampsia, there are steps you can take before and during pregnancy to decrease the chance of developing preeclampsia, under the guidance of your doctor.
- Overweight and obesity: If you were at an unhealthy weight before any pregnancy-related weight gain, losing weight can help decrease your preeclampsia risk. Tips for reaching and maintaining a healthy weight include eating a healthy diet and exercising regularly.
- High blood pressure: If you have high blood pressure prior to pregnancy, take steps to reduce it, such as by making dietary changes like lowering salt intake. Your doctor may also prescribe medication to help manage it.
- Diabetes: It’s important to control your blood sugar levels if you have diabetes. Some dietary changes can help manage diabetes as well as leading a healthy lifestyle.
Your doctor may recommend taking aspirin to help decrease the risk of developing preeclampsia. HRI is conducting further research to investigate the role of aspirin in preventing preeclampsia and prolonging pregnancy.
Preeclampsia treatment
Whether mild or severe, all forms of preeclampsia need to be treated. When preeclampsia is caught early, it can be treated and managed to keep both mother and baby safe and healthy. Treatment can include careful monitoring of blood pressure levels and medications to lower blood pressure and manage complications.
In mild cases of preeclampsia, you will be advised to have regular check-ups, and your blood pressure and urine will be tested regularly.
In severe cases, you may need to be admitted to hospital for closer monitoring and treatment, which may include rest and blood pressure or other medications. Hospital admittance may also be because the baby needs to be delivered as soon as possible.
The only cure for preeclampsia, and currently the main treatment if necessary, is a planned pre-term delivery of the baby. In some cases, it is safer for the mother and baby to deliver the baby early than to risk prolonging the pregnancy.
How is HRI fighting preeclampsia?
The Vascular Immunology Group at HRI focuses its research on better understanding the causes of preeclampsia, the condition’s impact on women during pregnancy, the impact on long-term cardiovascular health, as well as the development of new drug treatments for preeclampsia. Preventing preeclampsia is likely to have a positive impact on pregnancy outcome, and could help prevent or reduce the risk of future cardiovascular disease in women.
References
- Kuklina EV et al. Hypertensive Disorders and Severe Obstetric Morbidity in the United States. Obstet Gynecol 2009; 113:1299-306.
- Brown MC et al. Cardiovascular disease risk in women with pre-eclampsia: systematic review and meta-analysis. Eur J Epidemiol. 2013 Jan;28(1):1-19.
- Pearls: Preventing preeclampsia www.preeclampsia.org.au/index.html